
Back pain is a common problem among middle-aged and elderly patients. The cause of that can be an incorrect way of life, pathology of the musculoskeletal system, diseases of internal organs. A neurologist, orthopedist, nephrologist, and urologist can treat back pain, depending on their origin. It is difficult for the patient to discover the cause of unpleasant feelings on his own and to choose the right doctor. Therefore, it is initially necessary to contact a therapist who, depending on the symptoms, history and results of the studies performed, will refer you to a narrow specialist.
Classification
Back pain can be:
- Myofascial.
- Nociceptive.
- Neuropathic.
- Psychogenic.
Myofascial painobserved during the formation of the so-called. trigger points in the back muscles. Trigger points are pea-like nodules that form when muscles are constantly tense (when they simply cannot relax). Moreover, when one segment of a muscle fiber is compressed, the other is stretched. This affects the mobility of muscle fibers: it is limited. The fibers themselves shorten, become firmer.
Trigger points result from excessive muscle strain. Moreover, excessive stress can occur not only due to excessive physical activity, but also due to prolonged stay in one position (for example, sitting at a computer). Also, trigger points often occur in osteochondrosis.
Another factor that contributes to the formation of trigger points is the overstimulation of sarcomeres (basic contractile units that are a protein complex). If there is excessive stimulation of the sarcomeres, they are constantly in a contracted state.
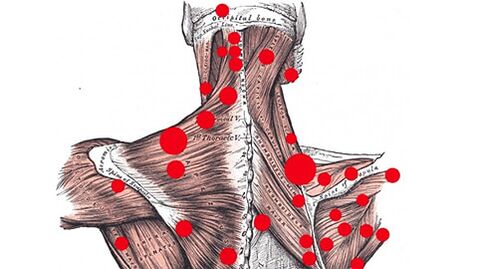
The presence of trigger points does not allow the muscle to relax completely. It starts to get tired quickly even with smaller loads, it moves overvoltage and recovers very slowly. Its limited range of motion affects the entire fascial chain. Other muscles and even some joints also become less mobile.
Blood flow in the tissues surrounding the trigger point also suffers. Therefore, oxygen starvation is observed in this area. Decomposition products accumulate, irritate the trigger point and therefore pain develops. In this case, the size of the muscles does not matter, it all depends on the degree of irritation of the point. Even the smallest muscle in the presence of trigger points in it can provide a lot of unpleasant sensations.
A characteristic feature of myofascial pain is their reflection. This means that the pain is reflected to other parts of the body. They can occur in areas very far from the trigger points. Thus, for example, pain may occur under the shoulder blades or in the lower back due to the presence of nodules in the abdominal muscles. Also, the lower back may ache due to trigger points in the calf area or in the buttocks.
Myofascial pain is usually long-lasting and dull. Sometimes they appear only in motion, sometimes at rest. The strengths can be different: from minor discomfort to unbearable pain.
Nociceptive pain- the body's reaction to direct irritation of pain receptors (nociceptors). In the case of the back, these are receptors located in the paravertebral ligaments, muscles, tendons, as well as in the articular capsules of the intervertebral joints and the outer third of the fibrous ring of the intervertebral disc. The patient may experience pain with reflex muscle spasm, dystrophic or pathological processes in the facet joints. When moving, the pain intensifies.
Neuropathic paindevelop in pathological processes in the nervous system: damage to nerves or roots of the peripheral nervous system, disorders of the central nervous system. Such pain can be noticed in osteoporosis, spondylolisthesis, hernia and spinal fractures. They intensify when bending, moving, straining, coughing, sneezing and in most cases are given to the limb. Sometimes they are annoying and painful, but more often they are sharp and shooting.
Psychogenic painthey occur due to muscle spasms caused by emotional stress, chronic stress, or anxiety disorder.
In some cases, the varieties can be combined with each other. For example, myofascial sensations coexist with nociceptive ones.
Also, back pain is divided into 3 types:
- Acute (lasts less than 6 weeks).
- Subacute (6-12 weeks).
- Chronic (more than 3 months).
Acute / subacute painit usually develops due to tissue damage (deep, superficial) due to cuts, wounds, inflammation. Therefore, the body warns us that something is wrong. The pain disappears after the tissues have completely healed.
Chronic painoccurs due to diseases of organs and systems or emotional disorders. If present, a thorough medical examination is necessary.
By location, the pain can be:
- Local.
- Reflected.
- Radiation.
Local pain develops directly at the site of development of the pathological process. Reflected - if there are trigger points. Radiation - with damage to internal organs, it spreads along nerve fibers.
Why does my back hurt?
Back pain can be caused by a variety of reasons, which include:
- Curvature of the spine: scoliosis, kyphosis.
- Neurological diseases: herniation of intervertebral disc herniation, osteochondrosis, spondylosis, spondyloarthritis.
- Endocrine pathologies: osteoporosis.
- Respiratory system diseases: pleurisy.
- Pathologies of the kidneys and urinary system: urolithiasis, pyelonephritis, glomerulonephritis.
- Tumors.
Short-term pain (usually severe, burning) can be caused by a variety of reasons. These include:
- Injuries.
- Excessive muscle strain (due to monotonous posture or performing the same types of repetitive movements).
- Hypothermia.
Pain caused by degenerative processes occurs in the following diseases:
- Osteochondrosis.
- Intervertebral hernia.
- Intervertebral disc protrusion.
- Spondylosis deformities.
- Degenerative scoliosis.
- Osteoarthritis.
- Spondylolisthesis (movement of the vertebrae).
- Spondylolysis (nonunion of vertebral arches).
- Spinal stenosis.
Pain radiating to the spine can develop due to the disease:
- Heart and large vessels: myocardial infarction, angina pectoris, aortic aneurysm.
- Lungs: cancerous tumors, pleuritis.
- Esophagus.
- Gallbladder and biliary tract: acute and chronic cholecystitis.
- Kidneys and urinary tract.
- Pancreas.
Back pain in rare cases can be of infectious origin. For example, sometimes my back hurts from the flu. Also, the infection can penetrate the spine from nearby organs: urinary system, kidneys.
Other reasons for the development of back pain may be changes in hormonal levels (for example, related to age, during or after menopause). In this case, hormonal spondylopathy occurs (degenerative changes in the spine)
Back hurts a lot: what to do?
If you have a severe attack of pain, be sure to see a doctor as soon as possible. However, if the sensations are so strong that any movement causes pain, first aid is needed. You must lie on your back on a flat, hard surface (for example, the floor). This will help relieve cramps, relax muscles and reduce pain.
When sinking on a flat surface, do not change the position of your back. Lying on your back, try to roll over on your side. This will relieve the spine. When the pain subsides, return to your back. It is recommended to put something under your feet, lifting them. Lie in this position for 10-15 minutes.
You also need to climb properly: roll over on your side first. From this position, go to all four. Then lean on something (if there is no support nearby - drag it to it) and get up slowly. Only then carefully straighten your back.
To find out why your back hurts so much, do not delay a visit to the doctor. This will help avoid new attacks.
Diagnosis
You should definitely make an appointment with a therapist if you have back pain:
- appear during physical exertion, muscle tension;
- last more than 3 days;
- are episodically repeated.
It is necessary to visit a doctor immediately in the following cases:
- back constantly sore;
- fever, numbness of the limbs, lethargy of the limbs in the morning are added to the pain;
- in the supine position the pain does not pass;
- the pain worsens at night.
At the meeting, the doctor will collect a medical history, examine the patient (assess the condition of the skin, body position and symmetry, gait, etc. ). They will then assign studies:
- general blood and urine analysis;
- X-ray;
- computed tomography;
- M. R. I.
If necessary, the therapist will refer the patient to a neurologist, orthopedist, urologist, gynecologist or nephrologist.
Treatment of back pain

Treatment for back pain is comprehensive and may include:
- taking medications (anti-inflammatory, pain medications, restorative medications);
- blockade (long-term pain relief);
- physiotherapy procedures;
- physiotherapy exercises;
- massages;
- manual therapy.
If conservative methods do not give the desired result, surgical treatment is prescribed. Modern methods enable the performance of low-trauma precision operations with a short rehabilitation period.
Prevention of back pain
Simple preventative measures can help prevent back pain. It is necessary:
- Track your posture.
- Sleep on a bed with a hard mattress.
- When engaging in activities that involve a long sitting position (driving, working at a computer), it is necessary to change your posture from time to time, as well as organize breaks and warm up.
- When you stand for a long time, lean on something.
- Do not wear high heels for more than 2 hours in a row.
- Spend time with moderate physical activity (swimming, fitness).
- Monitor your weight - back pain can occur due to the presence of extra pounds.
- Try not to lift weights.
- Do not turn or bend with sudden movements.
- Treat urological and gynecological diseases in a timely manner.
Preventive annual visits to a therapist will also be helpful. Pathologies identified in the early stages can be eliminated without waiting for complications to develop.






















